Abstract
Introduction: Red blood cell (RBC) transfusion remains a mainstay of treatment for both acute and chronic complications of sickle cell disease (SCD). RBC transfusions improve oxygen-carrying capacity of blood, decrease hemoglobin S levels, and are indicated for the treatment of complications such as stroke, acute chest syndrome, sickle cell hepatopathy and multiorgan failure syndrome. RBC transfusions may also be considered to reduce the frequency of pain crises for those intolerant or non-responsive to hydroxyurea. Prior practice surveys havedemonstrated significant practice variation in the management of patients with SCD with respect to RBC transfusions. The utilization of both simple RBC transfusions and red cell exchange (RCE) is poorly described, and unknown in the Canadian context, including at our center. The objective of this study is to describe RBC utilization at our center in a cohort of patients with SCD.
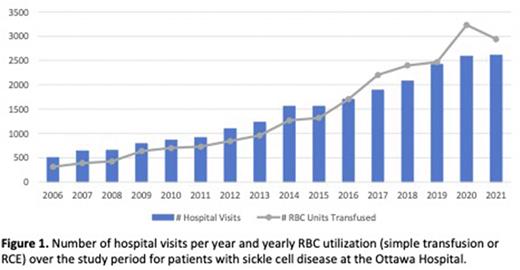
Methods: All adult patients with SCD who have received care [inpatient, outpatient, or emergency department (ED)] at the Ottawa Hospital, from January 2006 to May 2019 were identified for study inclusion. Transfusion and health care utilization data was obtained through to December 2021 from clinical, administrative and laboratory databases at the Ottawa Hospital.
Results: A total of 273 patients with SCD were identified. The median age for the cohort was 25 years (IQR 19,33) at first visit, with females comprising 53.9% of the cohort. The median duration of follow-up was 8.1 years (IQR 5,12.4). O-positive was the most frequent blood type (41.8%), and 8 (2.9%) individuals were O-negative. The annual RBC and health care utilization for the study cohort is depicted in Figure 1. The total number of hospital visits during the study period was 23127, with a median of 45 visits (IQR 18,100) per patient. 165 patients (60.4%) received 22538 RBC units with a median of 2 units (IQR 1,19) per patient, per year. 86.5% of the RBC units were infused in the outpatient setting, 12.1% in the inpatient setting and 0.8% in the ED. 40.3% of inpatient hospital visits were associated with an RBC transfusion event, compared to 2.4% of ED encounters. The proportion of RBC units transfused that were O-negative was 29.1% (6557 units). 147 patients received 2205 (9.7%) as simple RBC transfusions. The median number of simple RBC units transfused per patient, per year was 1 unit (IQR 1,2). 88 patients received 20333 RBC units during 2702 RCE sessions (median of 14.5 RCE sessions per patient), with 91.5% occurring in the outpatient setting. Of the 88 patients who received RCE, 64 patients (72.7%) had more than one RCE session, 54 patients (61.4%) had more than 5 RCE sessions and 48 patients (54.5%) had more than 10 RCE sessions. The median number of RBC units transfused per RCE session was 7 (IQR 6,9), with a median duration of 30 days (IQR 28,40) between RCE sessions.
Conclusions: RBC transfusion was common in our cohort, with the majority of patients having received at least one RBC transfusion. The largest proportion of transfused RBC units stem from RCE use, which represents a small proportion of on our SCD cohort. O-negative units represented a large proportion of units transfused, despite the predominance of non-group O patients, likely due to both differences in donor and patient blood group phenotypes, and recommendations for extended phenotype matching. With pressure on transfusion medicine to provide appropriately matched units and the scarcity of O-negative units, further data accrual on RBC utilization, particularly assessment of indications, requirements for matching, and review of RCE procedures will define further quality improvement interventions to ensure optimal utilization of RBCs.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.